 The human brain is an extraordinary and complex organ. It is responsible for our ability to think, feel, process information, concentrate, make decisions and experience emotions. It is responsible for our ability to walk, talk, eat, draw, write and sleep. It coordinates – without us even knowing it is happening – our breathing, heartbeat, organ function, blood circulation, digestion and more.
The human brain is an extraordinary and complex organ. It is responsible for our ability to think, feel, process information, concentrate, make decisions and experience emotions. It is responsible for our ability to walk, talk, eat, draw, write and sleep. It coordinates – without us even knowing it is happening – our breathing, heartbeat, organ function, blood circulation, digestion and more.
Unfortunately, traumatic brain injury is a major cause of death and disability in the United States. According to the Centers for Disease Control and Prevention (CDC), approximately 1.5 million Americans incur a traumatic brain injury, or TBI, each year. As a result of these injuries, each year in the U.S., 230,000 are hospitalized and survive, 50,000 die, and 80,000 to 90,000 are disabled.
A TBI occurs when a sudden bump, blow, jolt or penetrating head injury causes damage to the brain, which disrupts the normal function of the brain. TBI is very complex with a wide spectrum of signs, symptoms and impairments from the injury.
TBIs are the number one cause of death for people under the age of 45 years and the fourth leading cause of death for all ages. Nearly 30 percent of all injury-related deaths are the result of an injury to the brain. The risk of sustaining a TBI is highest among teens, young adults and those older than 75 years. The risk of sustaining a TBI is twice as high among males as it is among females.
TBI Signs and Symptoms
The symptoms of TBI can be seen immediately or can take days or even weeks to show up. A closed head injury or the absence of any external injury can be misleading and make diagnosis difficult. A severe or sudden hit to the head can cause the brain to bounce or ricochet back and forth inside the skull, which can be difficult to detect bleeding and bruising. Therefore, it is important to monitor a person for at least 24 hours after the hit or blow to the head to watch for symptoms of an injury. Two of the most common symptoms of TBI is depression and a change in vision (seeing double, blurred vision, decreases peripheral vision, lost sight in one or both eyes).
Other signs and symptoms include mood swings; uncommon feelings of sadness or anger; unexplained headaches; inability to concentrate or problem solve; nausea and vomiting for no reason; dizziness; seizures or convulsions; trouble communicating such as forgetting words or how to write/talk in complete sentences; clumsiness; and a decrease in hand-eye coordination and dropping items.
Recovery from TBI
Depending on the severity of the injury, TBI patients may need a few days or weeks of rest and limited activity. In more severe cases, rehabilitation therapy may be required. The goal of rehabilitation therapy, commonly called rehab, is to help patients regain their physical or cognitive (mental) abilities. Rehab may include physical, speech, occupational and behavioral therapies. The more severe the injury, the longer the recovery period. The longer the recovery period, the more long-term effects are likely.
There are several levels of rehab for TBI patients; not all patients need all levels:
Acute rehab focuses on many activities of daily living such as dressing, eating, using the bathroom, walking and speaking.
Post-acute rehab helps the patient become as independent as possible via three to six hours of therapy per day. This type of comprehensive rehabilitation in a post-acute rehabilitation hospital, such as the Rehabilitation Hospital of Northern Arizona, is considered the gold standard for care and treatment following brain injury.
Sub-acute rehab programs are designed for those who need less intense rehab but over an extended period of time. These patients have made progress in an acute and/or post-acute rehab hospital and are still progressing but are not making rapid functional gains. Sub-acute rehab is often provided in a skilled nursing facility.
Outpatient therapy usually follows rehab in a facility or is for those individuals whose injuries were not severe enough to require hospitalization or acute rehab. Outpatient therapies help the patient maintain and enhance his or her recovery.
TBI Rehabilitation in Northern Arizona
The highest quality rehabilitation care is available right here in Northern Arizona. The Rehabilitation Hospital of Northern Arizona, located on McMillian Mesa, is the only short-term acute-care inpatient rehabilitation hospital in the region. The Rehabilitation Hospital of Northern Arizona can help speed the recovery process following a TBI or other injury. Short-term rehab focuses on rebuilding strength, retraining muscles, regaining speech and rewiring the brain. Treatment plans are individualized and most patients participate in a minimum of three hours of physical and occupational therapy a day. FBN
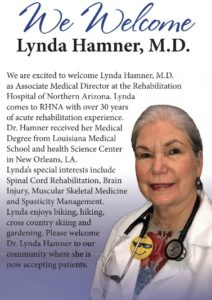
By Lynda Hamner, M.D.
The 40-bed rehabilitation hospital provides intensive rehabilitation services to people recovering from disabling diseases or injuries, such as strokes, brain, spinal cord and orthopedic injuries. For more information, visit rhna.ernesthealth.com or call 928-774-7070. Follow on Facebook at Rehabilitation Hospital of Northern Arizona.
Lynda Hamner, M.D., is the Associate Medical Director at the Rehabilitation Hospital of Northern Arizona. Dr. Hamner specializes in spinal cord rehabilitation, brain injury and muscular skeletal medicine.





